Putting sugar on a wound or cut will greatly reduce pain and speed up the healing process.
Sugar Actually Heals Wounds Faster (Science Confirms)
It sounds like something your grandmother would suggest after raiding the kitchen cabinet, but putting sugar on wounds is backed by serious medical research. Studies spanning decades—including a 2025 case report—confirm that granulated sugar accelerates healing, reduces pain, and fights infection when applied topically to cuts, burns, and ulcers.
The science is surprisingly straightforward. Sugar creates an osmotic effect that draws moisture out of the wound, which sounds counterintuitive until you realize this actually dehydrates bacteria and prevents them from multiplying. At the same time, it pulls fluid from surrounding tissue, reducing swelling and bringing the edges of the wound closer together.
The Sweet Science of Healing
Sugar doesn't just sit there being sweet—it actively promotes recovery through multiple mechanisms. It enhances the activity of lymphocytes and macrophages (your immune system's cleanup crew), provides an optimal environment for fibroblast growth (the cells that build new tissue), and even releases low levels of hydrogen peroxide that inhibit bacterial activity without damaging healthy cells.
Clinical studies report 89.5% satisfactory healing results when treating wounds with granulated sugar. In diabetic ulcer cases, healing times ranged from 9 days to 17 weeks, with an average of 5 weeks—impressive for wounds that typically struggle to heal.
Pain Relief You Can Taste (But Don't)
Here's where it gets interesting: sugar genuinely reduces pain, though not quite how you'd expect. When applied topically to burns and wounds, studies show it provides immediate pain relief—in some burn cases, eliminating the need for narcotic painkillers entirely. Sugar paste treatment for leg ulcers showed significant pain reduction alongside faster healing.
The pain-relieving effect differs from sugar's oral analgesic properties (which work through endogenous opioids in infants). For wounds, the mechanism likely involves the osmotic effect reducing pressure and inflammation in damaged tissue.
Not Your Average First Aid
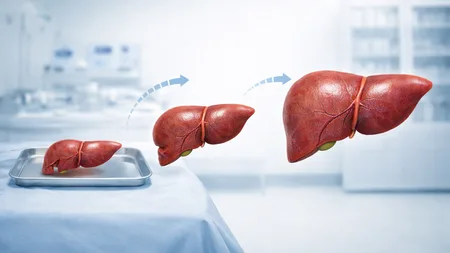
Before you ditch your Band-Aids for the sugar bowl, know that this treatment is typically used in clinical settings for chronic wounds, diabetic ulcers, and burns—not everyday paper cuts. The sugar needs to be granulated (not powdered), applied generously, and covered with a proper dressing. It's particularly valuable in resource-limited settings where advanced wound care products aren't available.
One important distinction: topical sugar helps wounds heal, but high blood sugar (hyperglycemia) does the opposite. Diabetics with poorly controlled glucose levels experience impaired healing—the sugar has to be on the wound, not in your bloodstream.
While honey appears slightly more effective in head-to-head comparisons, sugar remains a remarkably cheap and accessible treatment that produces reproducible benefits. A 2025 case study documented complete wound healing 21 days after starting sugar therapy—not bad for something that costs pennies and sits in your pantry.
Frequently Asked Questions
Does putting sugar on a cut really help it heal faster?
How does sugar reduce pain in wounds?
What type of sugar should you use on wounds?
Is sugar better than honey for wound healing?
Can diabetics use sugar on wounds?
Verified Fact
Extensive medical research confirms that topical sugar application promotes wound healing through osmotic effects, antimicrobial properties, and tissue growth stimulation. Recent 2025 case studies continue to document effectiveness. Sugar also provides pain relief when applied topically to wounds, with studies showing immediate pain reduction in burns and ulcers.
Related Topics
More from Body & Health